November 14th is World Diabetes Day! It is a personally relevant day for me as I am not only an endocrinology fellow but have been living with Type 1 Diabetes for 26 years. The day was not chosen at random – November 14th is the birthday of Sir Frederick Banting, a Canadian physician-scientist, who, along with his medical student, Charles Best, and others, discovered how to use insulin for therapeutic use in 1923. Unlike big pharmaceutical companies of today, Banting felt that insulin did not belong to him, but rather to those who need it – the hundreds of thousands living with diabetes. For that reason, he sold the patent rights for insulin to the University of Toronto for one dollar.
Insulin does not belong to me, it belongs to the world. – Sir Frederick Banting
Sample Diabetes Board Exam Practice Question
Before we dive in, test your type 1 diabetes knowledge by answering the following board review practice question from the BoardVitals Preventive Medicine Question Bank. You will find the answer and explanation at the end of this article:
Within what time frame should an initial screening examination for diabetic retinopathy be performed in a patient with type 1 diabetes mellitus?
A. At the time of diabetes diagnosis
B. 1 -2 years after diagnosis
C. 3-5 years after diagnosis
D. 7-10 years after diagnosis
The Magic of Insulin
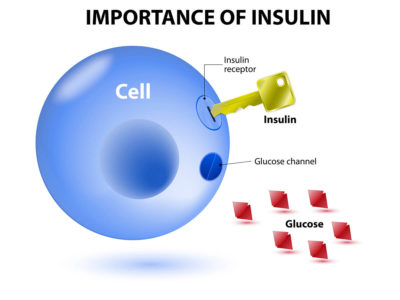
So…what is insulin? Insulin is a peptide hormone that is produced in the beta cells in the islets of Langherhans in the pancreas. Insulin secretion occurs in response to increases in serum blood glucose levels. After release into the bloodstream, insulin molecules bind to cellular transmembrane tyrosine kinase receptors, which trigger an elegant intracellular cascade, ultimately ending with intercalation of GLUT-4 receptors into the cell membrane, where they ferry extracellular glucose into the cell for use in ATP production. I like to envision insulin as a facilitator standing at the edge of the pier, hailing the ferry for the passenger (glucose) to hop aboard and get to its destination. In the absence of insulin, all of that glucose will remain in the blood (aka hyperglycemia). Hyperglycemia is the hallmark of diabetes.
In type 1 diabetes, the pancreatic beta cells are irrevocably destroyed by an autoimmune process. As a result, there is NO insulin production. Another function of insulin is suppression of lipolysis. In the absence of insulin, lipolysis of peripheral fat stores increases, due in part to increased hormone sensitive lipase activity. As a result, free fatty acids and glycerol are released into the bloodstream and ketoacids, including acetoacetic acid and beta-hydroxybutyric acid, are formed. Ketones provide an alternate energy source in the absence of glucose but will also lower the bloods pH. Ketogenesis can also lead to DKA, which can lead to death. Simply put, insulin saves lives, my own included. For that, I am eternally grateful to Dr. Banting and his team. Currently, insulin prices are skyrocketing and making the accessibility to this life-saving hormone inaccessible to far too many. This is a significant failure of our healthcare system and a problem that we must address.
Diabetes Management During Medical Training
I firmly believe that type 1 diabetes – or any medical condition – should never limit you. That said, it’s essential to take the necessary steps to ensure you can care for yourself in difficult situations. When I started medical school, I was very transparent to my colleagues, peers, and professors about what my diabetes would mean for me to fulfill my medical student duties. I had an irrational fear that if I needed to test my blood glucose during an exam or, worse, if I became hypoglycemic during an exam that my proctors and peers would assume I was cheating. At the start of every course, I would email my professor and my academic dean and explain my situation. I was very clear about my medical needs while also specifying things that I did NOT need (extra time, separate room, etc..), As long as I had access to my diabetic supplies during each exam and could snack if blood glucose levels dropped, I would be golden. My medical school was extremely accommodating, and in my pre-clinical years, I had a seamless assimilation into med student life.
Clinical rotations were more complicated. The unpredictable hours, stress, lack of sleep, and never knowing when or if I could find time to eat was difficult. I realized I needed a plan that I could implement in every rotation. I would also tell my senior resident and attending on the first day of each rotation that I had type 1 diabetes that would require me to test my blood glucose, adjust my insulin pump, and if necessary, step away to treat a low blood sugar. Everyone was incredibly understanding. Despite that, it is often challenging to be a medical student – lowest on the totem pole – and say to a superior that you need to scrub out to eat a snack. It feels… awkward. Looking back now, I see that not only did they not care, but self care and health maintenance is integral to your education and your care for your patients. As a resident with more control over my time, things became more manageable in some ways but also more difficult because my responsibilities increased (along with the stress). I have found that using a continuous glucose monitor (CGM) has been life-changing. A CGM allows me to continually track my blood glucose trends and readings. My CGM alarms when my blood glucose is heading high or low, which has saved me on more than one occasion when I’ve been passed out in the on-call room.
Lemons into (sugar-free) Lemonade
In many ways, my diabetes (while it sucks) has shaped my life in positive ways. I believe that if I had not been diagnosed in childhood, it’s very likely I would never have found my calling in medicine. Management of my diabetes taught me responsibility and complex physiology in a very real way at a very young age. Diabetes has had another unexpected benefit in my life. Often, when a patient has a chronic disease, it is easy for the patient not to feel as though the physician truly understands the day to day struggles they face. Knowing the struggles associated with a chronic disease personally and deeply allows me to better connect, understand, and help my patients.
Sample Diabetes Board Exam Question Answer & Explanation
Here’s the answer and explanation to the sample question from the BoardVitals Preventive Medicine question bank above:
Correct Answer:
C.3- 5 years after diagnosis
Explanation:
Initial retinopathy screening should occur within 3 to 5 years of diagnosis of type 1 diabetes and should occur at the time of diagnosis for type 2 diabetes. For either type, screening should be repeated every two years if there is no retinopathy present. In patients with retinopathy, annual follow-up exams are recommended. More frequent follow-up is recommended in patients with rapidly progressing retinopathy.
Reference: American Diabetes Association. Diabetic Retinopathy. Diabetes Care. 2002;25(suppl 1):s90-s93.
How did you do? Get more free practice questions to help you study for your board exams by signing up for a no-commitment free trial of any BoardVitals question bank today!