You’ve spent nearly your entire educational career taking multiple choice questions on exams. The ENT Oral Boards are a little different. It can be intimidating to go against conventional test-taking norms and take an oral exam. Between the unfamiliarity of the examination format and large body of information covered (encompasses 5 years of training) to the artificial setting of the examination, there are many factors that can increase your anxiety level.
Before you panic, keep in mind:
1. Be confident! You already know the material – you’ve been learning it for the last 5 years.
2. The test is not structured to make you fail; it is to make sure you are systematic, thorough, logical and are able to explain your actions, analyze the outcomes and manage the complications.
How can you best prepare for the ENT Oral Boards? Follow this advice in the days, months, and weeks before the exam to face the boards with confidence!
Months Before the Exam
Start using the same routine in the office and hospital setting. Chief complaint, relevant history of current presentation, past medical/surgical history (obstetric details in children), medications, allergies, social history, family history, review of systems and vital signs. Then perform a thorough physical examination and highlight the pertinent points. Review available data. Order studies which will either help you establish the diagnosis or change your management. Construct the differential diagnosis list, from most likely to least likely. Formulate the management plan. Same routine every time. Make it a habit.
Weeks Before the Exam
Go over common topics in Otolaryngology. Be familiar with common surgical complications and management of such. Review radiology images and pathology slides. Interpret audiograms. Be able to provide facial cosmetic analysis. Learn how to draw various flaps. Simulate cases with your contemporaries. Get used to talking and explaining your every question, decision-making step and management actions. Some time in the winter/early spring months you will have to review a rather long list of names and pick out clinicians you have ever interacted with to avoid being tested by familiar individuals.
Days Before the Exam
Get plenty of sleep. Eat well and stay well hydrated. Perform several checks to ensure that your internet is working smoothly. Select the right test day outfit. Don’t spend too much time cramming – you are not likely to retain new information, and will just continue to stress yourself out.
The Day of the Exam
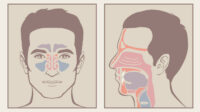
Have a good meal and be ready ahead of time. The ENT Oral boards are conducted in a virtual format, which allows you to choose a comfortable setting. Start your day off by having a good breakfast to keep your mind focused, and be ready to sign on at the time of your exam. Your proctor will keep track of time, so if he/she doesn’t want to go into details of family history, it means it is not important for the sake of time or not contributory. You may be given a picture of an imaging study, a pathology slide or a patient’s facial image. Describe what you see, even if you do not know what you are exactly looking at. After the review of clinical presentation and data, summarize your assessment. Present a solid differential diagnosis list, explaining why something is more or less likely. If you feel more information is needed, ask for it, but explain why.
Avoid asking for excessive and unnecessary tests. Narrow your differential and formulate a plan of action. In addition, other board-certified specialists offer the following tips:
- If there is a history of a “mass”, even benign – ask for the pathology report
- If there is a history of otologic or complex head and neck procedure – ask for the operative report and treatment records
- Counsel on smoking cessation
- Do not forget ancillary support – speech and language pathology, dental services, nutrition, social work
- Make sure your patients have proper follow up not only with you, but other specialties if needed (if there is an incidental diagnosis of an autoimmune process, refer the patient to the rheumatology)
- Always employ your reconstructive ladder (healing by secondary intention, primary closure, skin graft, regional flap, free flap)
- Provide proper prophylaxis to your patients (including tetanus)
- Remain calm and systematic, explain every step of your thought process
Still feel nervous about test day? Prepare for the ENT Oral Boards with practice questions from BoardVitals. The BoardVitals ENT Oral Boards Question Bank offers users access to 15 unique cases, with more than 50 review questions. Sign up for a free trial today!