There are pieces of good news and bad news in the 2017 Medscape Physician Compensation Report based on surveys from 19,000 physicians in 27 specialties. The information it delivers is just like the old rhyme about the little girl who had a little curl on her forehead, “When she was good she was very good and when she was bad she was horrid.” That’s what we have here; really good news and horrid news. Let’s jump in.
Here’s the good news:
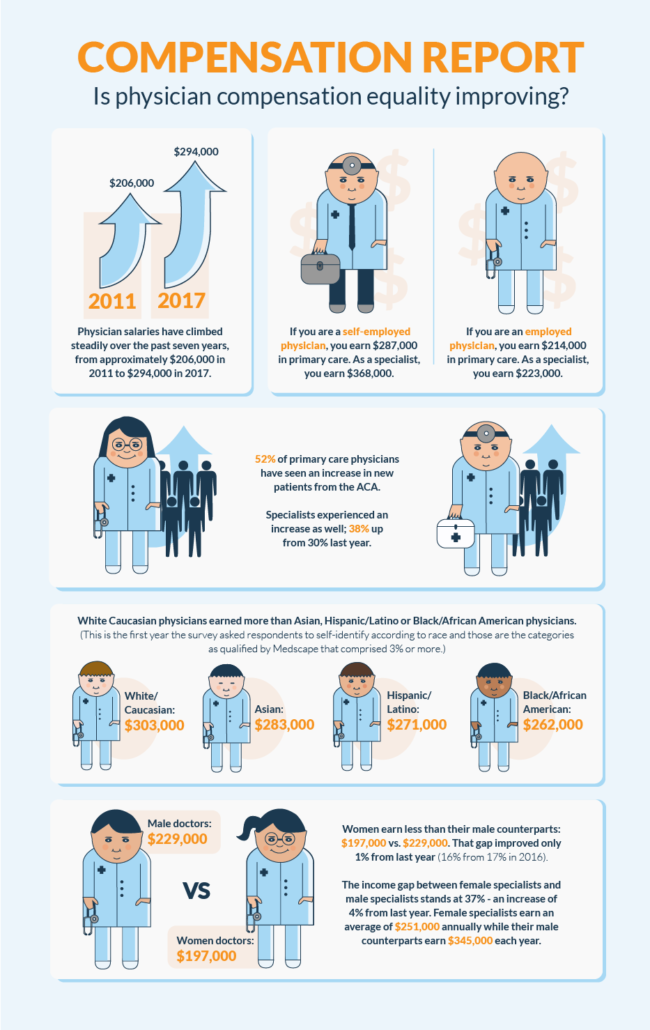
- Physician salaries have climbed steadily over the past seven years, from approximately $206,000 in 2011 to $294,000 in 2017. The climb is attributed to increased competition in the recruitment of physicians by hospitals, healthcare systems, urgent care centers and more.
- The majority of physicians receive benefits including health insurance (75%) and malpractice insurance (74%) from their employers and have not seen their income affected by the Affordable Care Act (45% of primary care and 42% of specialists).
- Two-thirds of physicians say that the most gratifying part of their job is the gratitude/relationship with patients and their skill at finding the right diagnosis.
- An overwhelming majority of physicians say they would choose medicine again. (71% was the lowest reported percentage among specialties- nephrologists).
- If you are a self-employed physician, you earn more than an employed physician. $287,000 vs. $214,000 in primary care. For specialists, it is $368,000 vs. $223,000.
- 52% of primary care physicians have seen an increase in new patients from the ACA. Specialists experienced an increase as well; 38% up from 30% last year.
- If you practice in North Dakota, Alaska, or South Dakota you earn more than your colleagues in any other state. ($361,000, $359,000 and $354,000 respectively.)
The bad news is very bad and if you are a primary care physician, a physician of color or a woman you might want to sit down.
- Specialists reported earning 46% more than primary care physicians. ($316,000 vs. $217,000).
- White Caucasian physicians earned more than Asian, Hispanic/Latino or Black/African American physicians. (This is the first year the survey asked respondents to self-identify according to race and those are the categories as qualified by Medscape that comprised 3% or more.)
- White/Caucasian: $303,000
- Asian:$283,000
- Hispanic/Latino: $271,000
- Black/African American: $262,000
- Women earn less than their male counterparts: $197,000 vs. $229,000. That gap improved only 1% from last year (16% from 17% in 2016).
- The income gap between female specialists and male specialists stands at 37% – an increase of 4% from last year. Female specialists earn an average of $251,000 annually while their male counterparts earn $345,000 each year.
- If you practice in Washington DC, Maryland, or Rhode Island/New Mexico, you earn less than your colleagues in other states. ($235,000, $260,000 and $261,000 respectively.)
- Bureaucratic tasks continue to contribute to physician burnout and it is getting out of control. Last year 35% of employed and 26% of self-employed physicians spent at least 10 hours a week on paperwork. This year 57% of physicians said they spend that amount of time on administrative work.
- 28% of physicians said numerous rules and regulations are the most challenging part of their job.
There are many more insights to be gained from the report conducted by Medscape. One of the most interesting may be behaviors that can result in leaking revenue:
- The number of physicians who say they either regularly or occasionally discuss the cost of treatments with patients declined significantly this year, down 10%. (75% from 85% in 2016).
- Most physician practices, an average of 72%, don’t charge for patient no-shows.
Last year we highlighted the yawning income gap between male and female physicians and it hasn’t improved. In 2016 we reported:
“Perhaps the most damning assessment of pay inequality comes from Jennifer Coombs, PhD, PA-C, assistant professor in the University of Utah Physician Assistant Program, published in Clinical Advisor in 2013. She calls the gender pay-gap “a discernible and persisting inequity”, saying that “Among physicians, for example, gender wage-gaps persist even after adjusting for factors such as full-time or part-time work, years in practice or specialty choice.”
We all need to work to close the income gap that continues to widen, whether it is between male and female physicians, or primary care physicians and specialists. Important headway needs to be made in pay equality and we will continue to keep a close eye on it for you.
The good news out of the survey is that you, as physicians, still believe in the mission of medicine. You are still deeply compassionate about your mission to care for the health and wellbeing of patients. That alone is reason enough for optimism and continued faith in the human race.