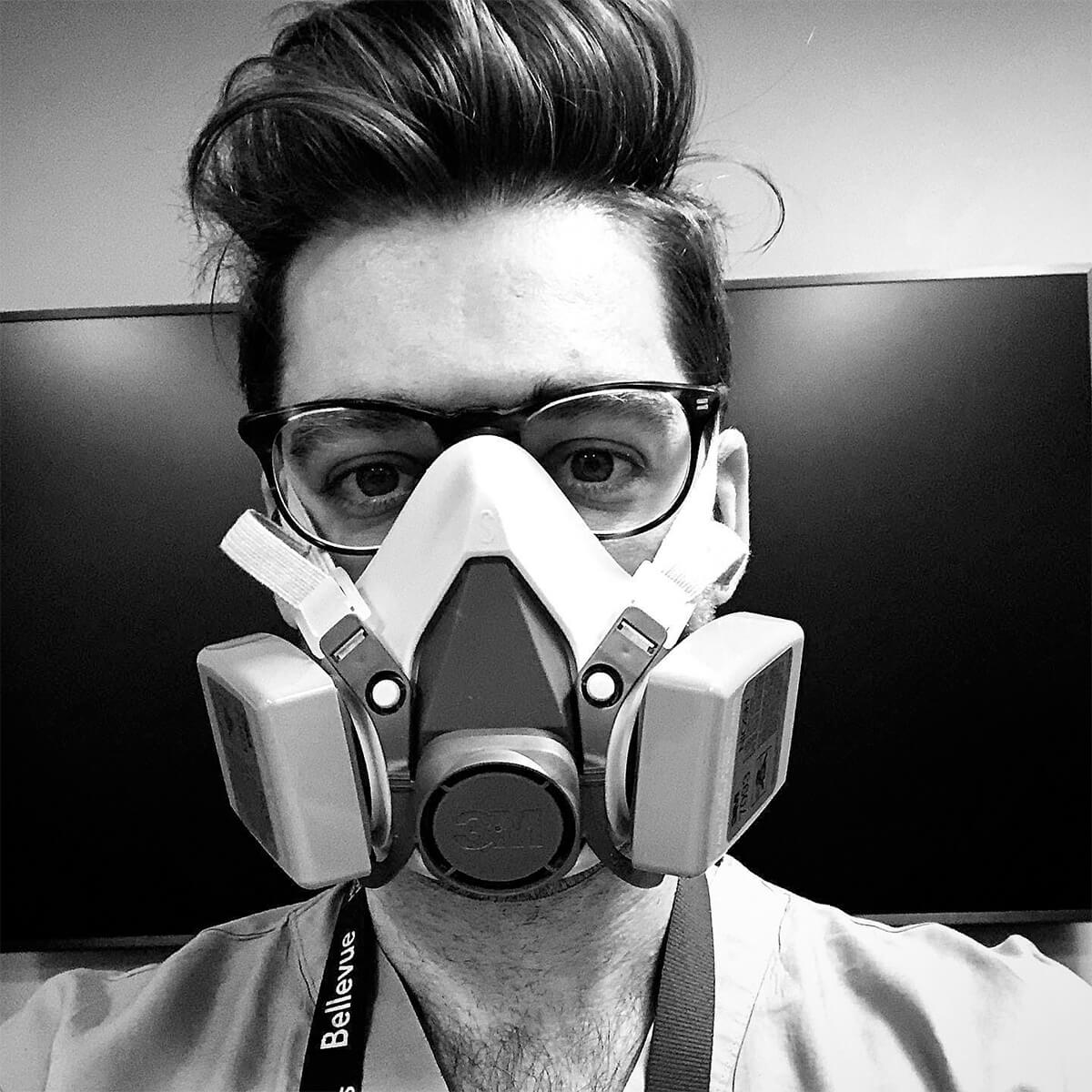
The world has changed. COVID-19 has disrupted every aspect of normalcy worldwide. Medical training during coronavirus has not been spared either. As a medical resident in a busy New York City hospital during this time, I can say first hand that I am seeing the necessary alterations that are constantly evolving in front of me.
How Hospitals Have Adapted to the COVID-19 Pandemic
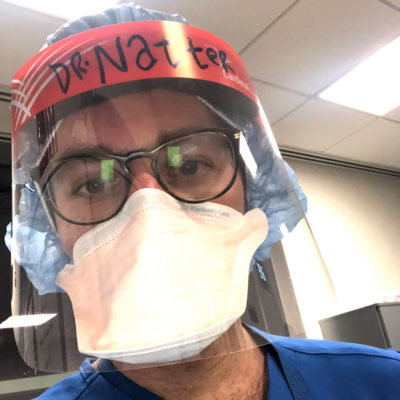 Prior to the pandemic, we would see a range of illness in the hospital with the bread and butter diseases (congestive heart failure, pneumonia, DKA, Cellulitis, etc) taking up the bulk of the volume. There was variety. There was range in severity and presentation. Now, upwards of 90% of the inpatient census is COVID-19, often with hypoxic respiratory failure. Besides the homogeneity of disease, there is also a massive surge in the overall volume of admissions. Hospitals are expanding their capacity by opening up previously dormant units or changing wards into intensive care level floors. We needed more clinicians and so many answered the call. Fellows and residents from non-medicine services stepped up. But another cohort did too, the fourth year medical students who graduated a few months early raised their hands to come join us on the frontline. These fluid changes and trying times have been daunting and honestly scary, but it also exposed the caliber and quality of my fellow healthcare workers. It inspired me to see those around me, stepping up, answering that call to arms.
Prior to the pandemic, we would see a range of illness in the hospital with the bread and butter diseases (congestive heart failure, pneumonia, DKA, Cellulitis, etc) taking up the bulk of the volume. There was variety. There was range in severity and presentation. Now, upwards of 90% of the inpatient census is COVID-19, often with hypoxic respiratory failure. Besides the homogeneity of disease, there is also a massive surge in the overall volume of admissions. Hospitals are expanding their capacity by opening up previously dormant units or changing wards into intensive care level floors. We needed more clinicians and so many answered the call. Fellows and residents from non-medicine services stepped up. But another cohort did too, the fourth year medical students who graduated a few months early raised their hands to come join us on the frontline. These fluid changes and trying times have been daunting and honestly scary, but it also exposed the caliber and quality of my fellow healthcare workers. It inspired me to see those around me, stepping up, answering that call to arms.
Past Memories of Similar But Different Times
In the late 1980s and early 1990s, house staff were faced with similar, albeit slightly different, circumstances. The HIV/AIDs epidemic was wreaking havoc amongst the population, namely in the densely populated urban centers. Hearing some attendings talk about their time as residents during that experience echoes much of what I was feeling at the start of this pandemic. Words like “fear,” “overwhelmed,” and “helpless,” were used. Whenever there is a widely communicable, invisible, incurable disease process that very little is known about, that barrier of intellectualization is no longer a defense mechanism. What if I get sick? My parents? My loved ones? My co-residents? Where is the textbook chapter on how to manage COVID? Why isn’t there an algorithm for how to treat it? A stockpile of potent antiviral agents? Despite all we do based on the little anecdotal evidence we have, the feelings of helplessness deepens.
Positivity During Dark Times
Yet, despite these dark times and narrow scope of illness we are seeing, medical training during coronavirus has its positives. For one, much of what I felt post 9/11 and what I imagined was felt by the American youth in the 1940s, was a deep-seeded urge to help. As medical residents, we are in a unique position to stand up and answer that call, to actually- potentially- directly help during this horrific time. Also, on a personal note, as I am only a short two months away from graduating from internal medicine residency, this pandemic has reinvigorated me as to why I became a doctor in the first place: to help those in need. The burnout has been rising in me and the finish line of residency could not have come soon enough, and then the world imploded. But it gave me the potent reminder of why I have worked so hard and sacrificed so much to acquire and hone this medical skillset. Now, more than ever, I am proud to be a medical resident.