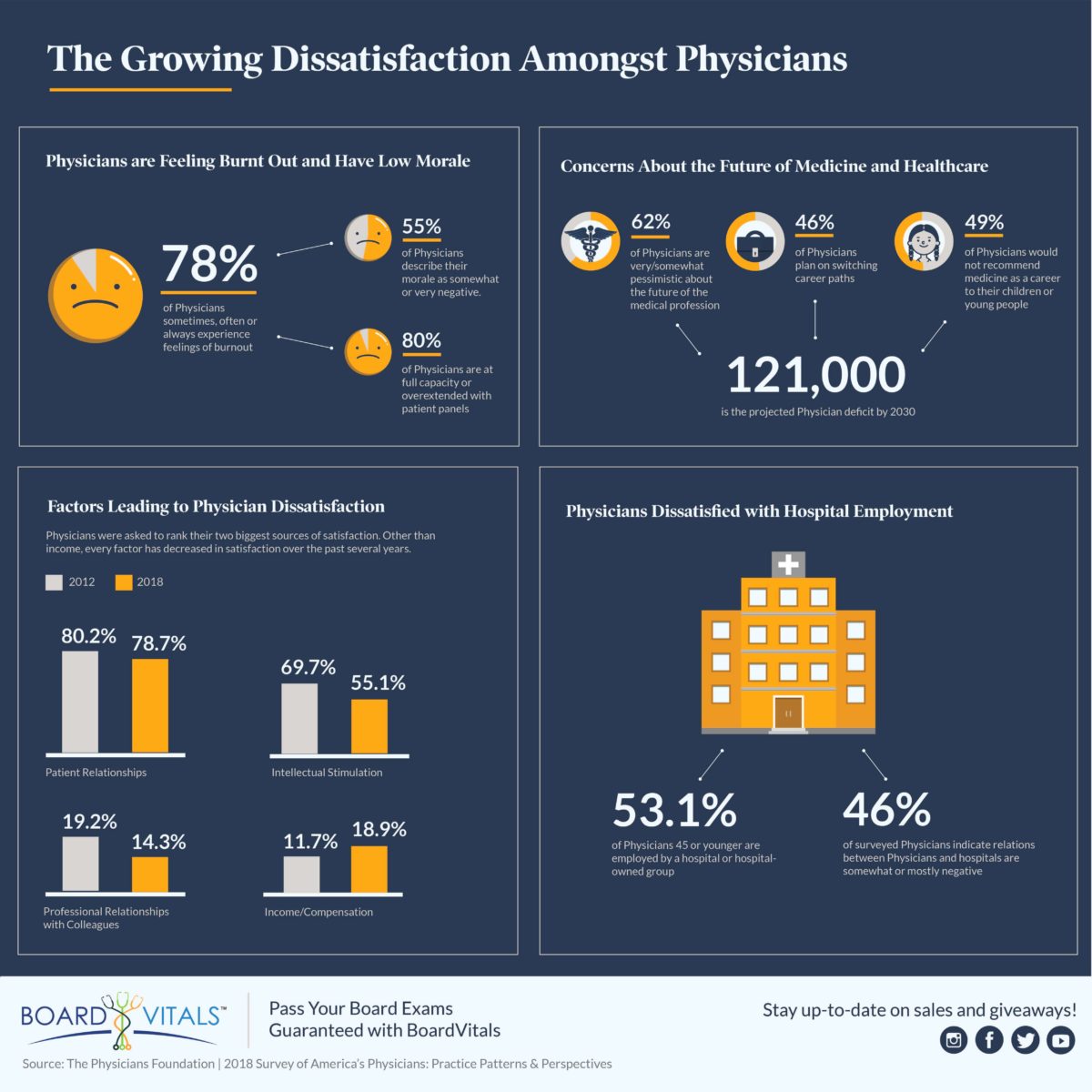
Every two years, The Physicians Foundation (TPF), with the assistance of Merritt Hawkins, conducts a survey of physicians across America to determine what they think about the state of healthcare today, their practice, access to care, and other critical issues. The 2018 Survey of America’s Physicians; Practice Patterns & Perspectives surveyed 8,774 employed and independent physicians across the country including family practitioners, general internists, and physicians specializing in other medical specialties. The results show that many physicians feel burned out and overextended and are pessimistic about the future of medicine.
Physicians’ Attitude on Practice and Perspectives in Healthcare
- 80% of physicians are at full capacity or overextended with patient panels
- 62% are pessimistic about the future of medicine
- 55% describe their morale as somewhat or very negative
- 78% sometimes, often or always experience feelings of burnout
- 23% of physician time is spent on non-clinical paperwork
- 46% plan to change career paths
- 47% of physicians have their compensation tied to quality/value, but only 18% believe quality/ value payments will improve care or reduce costs
- 49% would not recommend medicine as a career to their children
Based on the survey results, most physicians are feeling disgruntled or burnt out and are concerned about the future of medicine and the healthcare industry. The dissatisfaction has even led any physicians considering changing career paths.
Factors Leading to Physician Dissatisfaction
There are many factors leading to the growing dissatisfaction amongst physicians including being overextended with patient panels and time spent on non-clinical paperwork. The greatest source of professional dissatisfaction, however, is electronic health records. The survey asked, “What two factors do you find least satisfying about medical practice?” and here is how different factors increased or decreased since 2016.
EHR design/interoperability, dissatisfaction climbed:
- 2018: 39.2%
- 2016: 26.8%
Loss of clinical autonomy, dissatisfaction climbed:
- 2018: 37.0%
- 2016: 31.8%
Professional liability/malpractice, dissatisfaction climbed:
- 2018: 30.2%
- 2016: 23.5%
Regulatory/insurance requirements, dissatisfaction decreased significantly:
- 2018: 37.6%
- 2016: 58.3%
Amount of time with patients, dissatisfaction decreased:
- 2018: 12.4%
- 2016: 15.3%
Dissatisfaction with Hospital Employment of Physicians
Another major factor that contributes to physician dissatisfaction is the hospital employment of physicians.
- 57.5% of physicians do not agree that hospital employment of physicians is a positive trend likely to enhance the quality of care and decrease costs
- 46% of physicians indicate relations between physicians and hospitals are somewhat or mostly negative.
Despite their dissatisfaction, the majority of physicians are employed by either hospitals or large physician-practice groups, the result of mergers of multiple health systems. 53.1% of physicians 45 or younger are employed by a hospital or hospital-owned group, compared to 28.9% of physicians 46 or older.
Growing Physician Dissatisfaction
While physicians are increasingly satisfied with income/compensation, other critical factors have become increasingly less satisfying. When asked, “What two factors do you find most satisfying about medical practice?”, every other factor other than compensation has decreased in satisfaction. Here are the 2018 results compared to 2012.
Patient/physician relationship satisfaction has declined:
- 2018: 78.7%
- 2012: 80.2%
Intellectual stimulation has declined:
- 2018: 55.1%
- 2012: 69.7%
Professional relationships with colleagues; satisfaction has declined:
- 2018: 14.3%
- 2012: 19.2%
Professional stature of medicine; satisfaction has declined:
- 2018: 9.8%
- 2012: 10.0%
Income/compensation satisfaction has increased:
- 2018: 18.9%
- 2012: 11.7%
Risky Dissatisfaction
These aren’t just numbers on a page. America is facing a potential shortage of more than 121,000 physicians by the year 2030 due to the growing dissatisfaction of the healthcare industry and overall physician lifestyle. If physicians are burned out, looking to change careers, and not recommending medicine to others, that doesn’t bode well for educating new physicians to fill the gaps.
At the very same time that the country faces a physician shortage, it is also experiencing exponential growth in aging patients. Fewer physicians and more patients is not a workable equation.
A potential physician shortage is especially concerning because the country is also facing exponential growth in aging patients.
- By 2030, the population 65 and older will grow by 55%
- People 65 and older represent 14% of the population but account for 34% of inpatient procedures and 37.4% of diagnostic tests and treatments
- Older people see a physician at three times the rate of younger people
As physician morale decreases, so does their level of activity in the profession. Some may begin to limit practice hours, see fewer patients, or leave the active practice altogether in favor of management or teaching positions. It serves to limit access for patients, at a time when increased access is desperately needed. While more than 55% of physicians report feeling “somewhat or very negative” about the medical profession, only 15% of people in the general workforce feel the same about their jobs.